FREQUENCY OF OCULAR COMPLICATIONS OF LEPROSY IN INSTITUTIONALIZED PATIENTS IN NWFP PAKISTAN
Tajamul Khan, Abdul Aziz Awan*, Hasan Sajid Kazmi*, Ashfaq Ali Shah*, Sardar Muhammad, Shad Muhammad**
Departments of Ophthalmology Ayub Teaching Hospital, *Ayub Medical College Abbottabad, and Lady Reading Hospital, Peshawar
Background: There is no systemic disease, which so frequently gives rise to disorders of the eye as leprosy does. The study was conducted to determine the prevalence and gravity of ocular complications in institutionalized leprosy patients in NWFP. It is important to provide necessary information to leprosy health workers and general physicians in order to sensitize them to early detection and treatment or referral to appropriate centre. Methods: A prospective study of ocular complications of leprosy patients was conducted at the leprosy centre of Lady Reading Hospital Peshawar and the Leprosy Hospital Balakot, district Mansehra. The study included a record of the name, age, sex, type, duration of disease and completion of multi-drug therapy (MDT). Classification of the patients was done according to Ridley and Jopling 5-group system. Visual acuity was tested by Snellen chart and those patients having a vision of less than 3/60 were labelled as blind. Ocular adnexa were examined by naked eye and lacrimal sac regurgitation test was done. Slit lamp biomicroscopy was done for anterior segment examination and direct ophthalmoscope was used for fundoscopy. Results: The authors studied 143 patients in the above mentioned leprosy centres. Out of these, 59 had lepromatous leprosy, 39 borderline tuberculoid leprosy, 9 tuberculoid leprosy, 33 borderline lepromatous leprosy, and 33 borderline leprosy. The majority of patients came from the northern districts of NWFP, including Malakand division and district Mansehra. The male to female ratio was 4:1. The age of the patients ranged from 14 to 80 years and the duration of the disease ranged from 1 year to 48 years. Ocular complications were found in 73 % of the patients. These complications included loss of eyebrows in 57 patients, loss of eyelashes in 37, corneal changes (including opacity, ulceration, and/or anaesthesia) in 44, iridocyclitis in 31, lagophthalmos in 36, ectropion in 13, and chronic dacryocystitis in 3. Of the total of 15 (11%) patients who went blind from ocular complications, 16 eyes did so due to corneal opacities, 6 eyes due to cataract, 5 eyes due to chronic anterior uveitis and one eye due to corneal ulcer, panophthalmitis and phthisis bulbi each. Conclusions: A significant number of leprosy patients (73%) have ocular complications. The frequency of ocular complications increases with the increasing age and duration of disease of the patients.
INTRODUCTION
Leprosy is a chronic granulomatous disease caused by the intracellular acid-fast bacillus Mycobacterium leprae, whose clinical manifestations are largely confined to the skin, peripheral nervous system, upper respiratory tract, eyes, and testes 1.
It is a disease that does not kill the affected individual but cripples. It is not rare but rarely seen; this is due to the stigma attached to the disease causing the patients to hide their ailment and the doctors to ignore and neglect the disease. The number of leprosy patients in the world in 1991 had been estimated at 10–12 million and the number of individuals with deformities as between 2 and 3 million2; but after the introduction of MDT worldwide there are approximately 1.5 million leprosy patients taking multi-drug therapy. It is estimated that 1.5–2 percent of the total are blind from leprosy related causes and another 2 percent are blind from non-leprosy causes 3.
It is a systemic disease with the highest incidence of ocular complications 4. Mechanism of ocular involvement may be either due to invasion of the eyeball from adjacent skin lesions, or haematogenous spread, or involvement of the branches of the facial or corneal nerves, contributing to exposure keratitis.
For simplicity, ocular lesions can be classified into two groups. The first group is called potentially sight threatening lesions and the second group as academic lesions. Potentially sight threatening (PST) lesions comprise lagophthalmos and its sequelae, corneal hypoaesthesia and its sequelae, chronic iridocyclitis and its sequelae and scleritis. Academic lesions, such as loss of eyebrows and eyelashes, have no visual significance but contribute to the stigma which these patients endure5.
According to Ridley and Jopling 6 the classification of leprosy patients can be regarded as a spectrum determined by the cell-mediated immunity of the individual. Patients are either paucibacillary (smear negative) usually indeterminate, tuberculoid (TT) and borderline tuberculoid (BT) type or multibacillary (smear positive), usually borderline lepromatous (BL) or polar lepromatous (LL) type but detailed classification indicates prognosis.
Generally in tuberculoid, borderline tuberculoid, and mid borderline cases, damage to the eye is caused indirectly by M. leprae either secondary to motor or sensory nerve damage. In lepromatous leprosy and borderline leprosy eye is damaged due to infiltration by M. leprae, which takes years for destruction of various tissues of the eyes. But the type 1 and type 2 leprosy reactions encountered during the course of the disease, cause ocular involvement within days. Type 2 reactions usually cause acute iridocyclitis. Type 1 lepra reactions usually cause involvement of the ophthalmic division of the trigeminal nerve and the zygomatic and the temporal branches of the facial nerves 1.
Eye involvement in leprosy is quite common and its complications, particularly potentially sight threatening lesions, if neglected, will lead to blindness 10. Good vision is required not only for the performance of routine activities but also for the care of anaesthetic hands and feet. Loss of eyesight in a person who already have anaesthesia in hands and feet is a disaster. The main objective of the study was to observe the frequency and gravity of these complications in relation to the type of leprosy, and to determine the geographic distribution of these patients.
MATERIAL AND METHODS
One hundred and forty-three patients were examined at the Leprosy Centre of Lady Reading Hospital Peshawar and the Leprosy Hospital Balakot district Mansehra between August 2001 and August 2002. In each case name, age, sex, address and duration of disease were noted. The patients were classified in to five groups according to Ridley and Jopling 6. The ocular examination included testing of visual acuity by Snellen chart, macroscopic examination of eyebrows, lids, conjunctiva and sclera. The cornea, anterior chamber, iris and lens were examined by slit lamp examination. Fundoscopy was done with direct ophthalmoscope. The corneal sensation was tested with a wisp of cotton wool. For the purpose of this study blindness was recorded if the visual acuity was less than 3/60 in the better eye. The function of facial nerve was tested.
RESULTS
In our study a total of 143 leprosy patients were examined for ocular complications. One hundred and thirteen (72%) patients were male while 30 (28%) patients were female (Figure 1).
Figure-1: Distribution of 143 leprosy patients according to the sex and type of the disease.
LL : lepromatous leprosy. BL: Borderline lepromatous. BB: Mid borderline BT: Borderline tuberculoid TT: Polar tuberculoid.
The age of the patients varied between 14 years to 80 years (Figure 2).
Figure 2: Distribution of 143 leprosy patients according to age (years) and sex.
The duration of disease ranged from 01 year to 48 years. Among these 105 patients (73%) had ocular complications. The various complications observed are presented in Table 1. Blindness occurred in 15 (11%) patients. Out of the 30 eyes of blind patients the cause in 16 eyes was corneal opacification (53%), in 6 eyes cataract (20%), in 5 eyes chronic anterior uveitis and in one eye each a corneal ulcer, panophthalmitis and phthisis bulbi.
Table-1: Frequency of ocular
complications according to the type of leprosy.
LL: lepromatous leprosy BL: Borderline lepromatous BB: Mid borderline BT: Borderline Tuberculoid TT: Polar Tuberculoid.
|
|
Type of Leprosy / No of patients |
|||||||||||
|
Eye Lesions |
LL |
BL |
BB |
BT |
TT |
Total |
||||||
|
59 |
33 |
3 |
39 |
9 |
143 (100%) |
|||||||
|
Loss of eyebrows |
39 (66%) |
13 (39.4%) |
0 |
3 (7.7%) |
2 (22%) |
57 (40%) |
||||||
|
Loss of eyelashes |
23 (39%) |
8 (24%) |
0 |
4 (10.25%) |
2 (22%) |
37 (26%) |
||||||
|
Lagophthalmos |
14 (24%) |
7 (21%) |
1 (33%) |
11 (28%) |
3 (33%) |
36 (25%) |
||||||
|
Ectropion |
5 (8.5%) |
2 (6%) |
1 (33%) |
4 (10%) |
1 (11%) |
13 (9%) |
||||||
|
Defective blink |
1 (1.7%) |
2 (6%) |
1 (33%) |
1 (2.6%) |
0 |
5 (3.5%) |
||||||
|
Chronic Dacryocystitis |
1 (1.7%) |
0 |
0 |
2 (5%) |
0 |
3 (2%) |
||||||
|
Chronic Conjunctivitis |
19 (32%) |
11(33%) |
1 (33%) |
11 (28%) |
1 (11%) |
43 (30%) |
||||||
|
Corneal opacities |
16 (27%) |
6 (18%) |
0 |
2 (5%) |
2 (22%) |
26 (18%) |
||||||
|
Corneal ulcers |
2 (3.4%) |
0 |
0 |
0 |
0 |
2 (1.4%) |
||||||
|
Exposure keratitis |
6 (10%) |
3 (9%) |
0 |
4 (10%) |
3 (33%) |
16 (11%) |
||||||
|
Chronic Iridocyclitis |
17(29%) |
5 (15%) |
0 |
5 (13%) |
1 (11%) |
28 (20%) |
||||||
|
Acute Iridocyclitis |
3 (5%) |
0 |
0 |
0 |
0 |
3 (2%) |
||||||
|
Episcleritis |
1 (1.7%) |
0 |
0 |
0 |
0 |
1 (0.7%) |
||||||
Regarding different regions from where these patients came, the majority of the patients belonged to Malakand division and district Mansehra as shown in Fig-3.
Figure-3: Geographic distribution of 143 leprosy patients examined
DISCUSSION
The study shows a male to female ratio of 4:1. This preponderance of male patients has also been observed in India and one reason given is that males in general expose themselves to greater risks of infection as a result of their lifestyle 5.
On the other hand women may tend not to seek medical help even when it is required. Majority of the patients were “Multi-drug therapy” treated but the present study shows ocular complications in 73% having a close similarity with the study already conducted in Nepal 1 which is 74.2%. Potentially sight threatening lesions were found in 49% patients at Peshawar while these lesions were found in 40% patients at Balakot. The relatively better situation at Balakot is due to inclusion of the patients residing in leprosy colony while all the patients examined at Peshawar were admitted in the ward for the treatment of systemic or ocular complications. Patients with PST lesions deserve special care and follow-up as these lesions ultimately lead to blindness 3.
The loss of eyebrows was the commonest complication in lepromatous leprosy. It was observed in 66% of LL type, 39% of BL type and 7% of BT type patients. Loss of eyebrows is a cosmetic blemish, but may be a useful clue to other ocular complications in lepromatous leprosy (Figure 4).
Fig-4: Loss of eyebrows in a patient with LL
![]()

Uveitis, which has been described as an insidious cause of blindness 3, occurred most commonly in patients with lepromatous type of leprosy. It was found in 34% of LL and only 13% of BT type patients. Eighty-five percent of these patients were suffering from chronic anterior uveitis while only 15% had acute anterior uveitis. Chronic anterior uveitis presented in the form of chronic miosed pupil, posterior synechiae and iris atrophy. Ffytche 9 has suggested that chronic iritis in leprosy is more of a neuroparalytic origin than due to true inflammation. Chronic uveitis can lead to the development of cataracts, glaucoma, or macular oedema 1 (Fig. 5).
Fig-5: Miosed pupil due to chronic anterior uveitis

Corneal opacities, which presented as one of the major causes of blindness and visual impairment, were found in 18% of the patients as compared to 7% reported in another study of institutionalized patients from Nepal 7.
Corneal hypoaesthesia, seen in 18% of our patients, is a potentially serious complication of ocular leprosy and is secondary to trigeminal nerve damage. It may be seen in all forms of leprosy. Our finding is almost similar to a study at Rawalpindi which showed corneal hypoaesthesia in 21% patients10. There are several ways in which corneal hypoaesthesia can lead to the development of infectious keratitis and its sequelae: (a) injuries to the cornea can often be ignored or go unnoticed for a significant period of time (b) intact corneal sensation is also an important factor in tear production therefore patients are at risk of developing dry eye (c) when hands are deformed, callous, or ulcerated with poor sensation, they can easily injure an itchy eye with decreased corneal sensation (d) decreased corneal sensation can also retard the healing of corneal ulcers. Normal corneal sensation is essential for the proper maintenance of an intact corneal epithelium, so healing of an infectious keratitis in a leprosy patient with impaired corneal sensation is likely to be prolonged, difficult, and the end results not very rewarding 11.
Another sight-threatening complication is lagophthalmos, which was found in 25% of our patients which is similar to a study conducted at Rawalpindi 10 It leads to exposure of the cornea, micro traumata, secondary infections and ultimately progressive opacification of the cornea.12 (Figures 6 & 7)
Fig-6: Bilateral tarsorrhaphy done for a patient with bilateral lagophthalmos (open eyes)
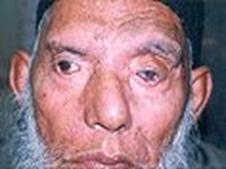
Fig-7: Bilateral tarsorrhaphy done for a patient with bilateral lagophthalmos (closed eyes)

Blindness was seen in 11% of the cases as compared with 9% and 12.7% observed by Akbar et al 10 and Malla et al 7 respectively.
Most of the patients were from Northern districts of N.W.F.P. especially the districts of Malakand division and Mansehra. The climate is cold in these areas, poverty is rife and the living conditions are unhygienic. Family history was positive for leprosy in 5% patients, while Akbar et al10 have reported a figure of 21%.
CONCLUSIONS
Peripheral neuropathy and ocular complications are common and severe in leprosy patients after they are cured mycobacteriologically. As ocular compli-cations are potentially sight threatening and lead to blindness as it is 11% in our study, it is recommended that these patients should be regularly followed up by an ophthalmologist in eye O.P.D.
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the cooperation of the staff of Leprosy Centre of Lady Reading Hospital Peshawar and Leprosy Hospital Balakot-Mansehra. Thanks are also due to Dr. Ruth Pfau and Dr. Thomas J Chiang of Mary Adelaide Leprosy centre Karachi, and Dr. Chris Schmotzer of Aid to Leprosy Patients Rawalpindi for providing important literature about leprosy.
REFERENCES
1. Gelber RH. Leprosy. In : Braunwale E, et al (eds) Harison’s Principles of Internal Medicine-1, 15th ed. McGraw-Hill, New York 2001: 1035
2. Noordenn SK, Brvo LL, Daumerie D. Global review of multi drug therapy (MDT) in leprosy. Wld Hlth Statist Quart; 1991;44
3. Lewallen S, Narong C, Tungpakorn, Kim SH, Courtright P. Progression of eye disease in “ cured “ Leprosy patients: implications for understanding the pathophysiology of ocular disease and for addressing eye care needs. Br J Ophthalmol 2000; 84: 817-821.
4. Kanski JJ. Clinical Ophthalmology, 4th ed. Butterworth-Heinemann Oxford Auckland Boston Johannesburg New Delhi 2001: 293-294.
5. Lamba PA, Santoshkumar D, Arthariswaran R. Ocular Leprosy-a new perspective. Indian J Lepr 1983; 55: 490-5.
6. Ridley DS, Jopling WH. Classification of leprosy according to immunity, a five group system. Int J Lepr 1966; 34:255-73.
7. Malla OK, Brandt F, Anten JGF. Ocular findings in leprosy patients in an institution in Nepal (Khokana). Br J Ophthalmol 1981; 65:226-230.
8. Espiritu CG, Gelber R, Ostler HB. Chronic anterior uvietis an insidious cause of blindness. Br J Ophthalmol 1991; 75:273-275.
9. Ffytche FJ. Role of iris changes as a cause of blindness in lepromatous leprosy. Br J Ophthalmol 1981; 65:231-139.
10. Akbar MK, Baig MA, Khan MA. Ocular involvement in various types of leprosy. Pak Armed Forces Med J 1998; 48(1): 11-14.
11. John D, Daniel E. infectious keratitis in leprosy. Br J Ophthalmol 1999; 83: 173-176.
12. Hwgweg M, Faber WR. Progression of eye lesions in leprosy: ten-year follow-up study in the Netherlands. Int J Lepr Other Mycobact Dis 1991; 59: 392-397.
Address for correspondence:
Dr. Tajamul Khan, Senior Registrar, Department of Ophthalmology, Ayub Teaching Hospital Abbottabad.